
avenger
Resource on self-management
Refer to expert solutions on mosquito disease diagnosis and treatment
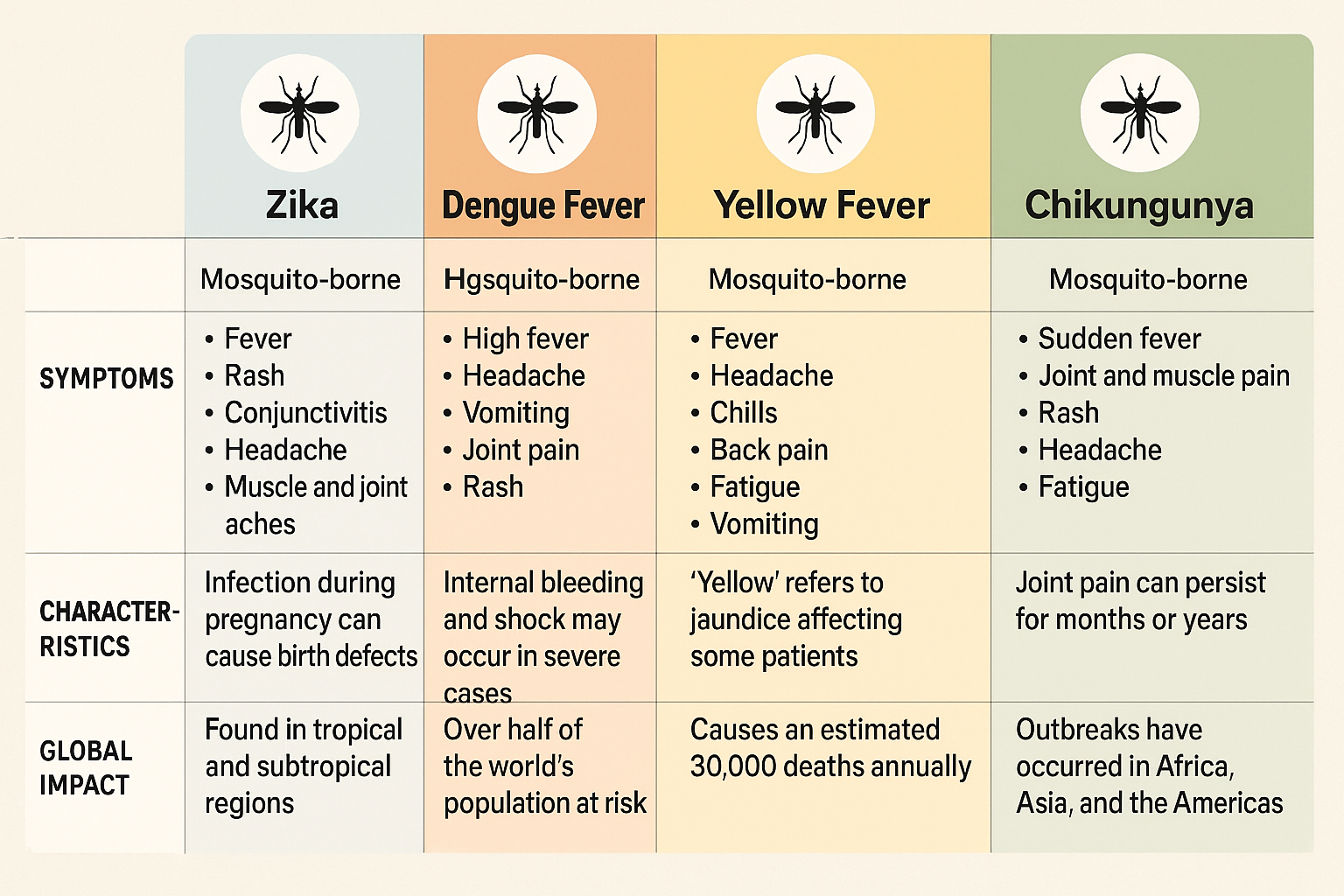
Common types of mosquito-borne diseases
Common types of mosquito-borne diseases include malaria, dengue, West Nile virus, chikungunya, yellow fever and Zika.
Below comparison highlights diagnostic and management challenges in regions with co-circulation and co-infected of these viruses.
Key questions and answers
What is the treatment for dengue?
Treatment for dengue fever is supportive; no specific antiviral therapy is available. Patients are advised to rest, maintain adequate fluid intake, and consult healthcare professionals. Paracetamol may be used for fever and pain relief, while medications like aspirin or ibuprofen should be avoided, as they elevate bleeding risk.
During the infectious period (typically 4−5 days after symptoms, up to 12 days maximum), infected individuals can transmit dengue via Aedes mosquitoes. Preventive steps include sleeping under insecticide-treated nets, especially while febrile, to minimize mosquito exposure.
Immunity after infection is strain-specific, providing lifelong protection only against that strain. Subsequent infection by other strains may still occur, potentially progressing to severe dengue.
If warning signs of severe dengue develop, prompt medical attention and possible hospitalization are crucial for disease management. With timely care, mortality rates are very low (less than 1%), though the illness itself remains highly uncomfortable.
What should I do if I suspect I have dengue?
If you suspect dengue infection, promptly consult a doctor. For diagnosis, your physician will:
• Assess your symptoms
• Order blood tests to detect dengue virus
• Review your medical and recent travel history
Anyone who has visited dengue-endemic regions within the last two weeks should inform their doctor.
Is there a dengue vaccine?
Currently, only one vaccine is licensed for dengue prevention: TAK-003.
TAK-003 is administered as a two-dose series, three months apart, for select age groups under specific circumstances as recommended by WHO.
WHO advises using TAK-003 in children aged 6–16 years in areas with high dengue transmission.
Dengue vaccination should be part of a comprehensive disease control approach, including vector control measures, effective case management, community education, and engagement.
How is chikungunya diagnosed?
Diagnosing chikungunya by symptoms alone is challenging, as they closely resemble those of dengue and Zika.
Laboratory tests are necessary to confirm infection.
• In the first week of illness, chikungunya can be identified by detecting the virus in blood samples using molecular methods or virus isolation
• After the initial week, blood tests for antibodies can confirm recent or past infection, typically performed 1 to 2 weeks apart
Accurate diagnosis is essential, especially in regions where similar viruses circulate.
Is there a vaccine for chikungunya?
Currently, two single-dose chikungunya vaccines—IXCHIQ and VIMKUNYA—have been approved by regulatory authorities in several regions, including the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA).
These vaccines are typically recommended for individuals at higher risk of severe chikungunya and for travelers to areas with active transmission. However, global availability and usage remain limited.
How can I protect myself and my family from mosquito-borne diseases ?
Prevention is the most effective strategy to protect yourself and your family. Key measures include
• Applying mosquito repellent (with DEET, IR3535, or picaridin) to exposed skin or clothing as directed
• Wearing protective clothing, such as long sleeves and trousers, especially during daylight hours when chikungunya-transmitting mosquitoes are most active
• Sleeping under mosquito nets, particularly during the day
• Installing mosquito screens on doors and windows, or keeping them closed, to prevent mosquitoes from entering indoors
• Removing standing water from items like tires, buckets, and flowerpots, as these serve as common mosquito breeding sites
What can be done to reduce the risk of mosquito-borne diseases ?
The most effective way to prevent Aedes mosquito-borne diseases is source reduction—eliminating mosquito breeding sites. By minimizing eggs, larvae, and pupae, the number of adult mosquitoes and the risk of disease transmission are decreased.
Typical mosquito breeding habitats include:
Indoors:
• Ant traps
• Flower vases and saucers
• Water storage tanks (domestic, bathroom)
• Plastic containers
• Bottles
Outdoors:
• Discarded bottles and tins
• Used tires
• Artificial containers
• Tree holes, potholes, construction sites
• Rainwater drums
• Tree shells, husks, pods
• Plant leaf axils
• Boats and equipment
Items that collect or store water should be covered or disposed of properly. Essential containers should be emptied, cleaned, and scrubbed at least once per week to remove mosquito eggs. This interrupts the mosquito life cycle and stops adults from emerging.
Active community involvement is crucial. When households collectively reduce mosquito breeding sites, vector density and disease transmission rates can be significantly lowered or eliminated.